Signs and Stages of a Pressure Ulcer
Signs of a pressure ulcer developing can first be seen when the area on the patient’s skin in contact with the device becomes red and warm to the touch. There are four progressive stages as shown below:
A pressure ulcer, also known as a pressure sore or pressure injury, refers to localised damage to the skin and the underlying tissues. These ulcers usually appear on thin tissue covering bony parts of the body that are in contact with hard surfaces such as a bed or a medical device.1
When fitted with a medical device such as a mask or breathing tube for long periods of time, patients are at an increased risk of developing a pressure ulcer. These may cause pain, anxiety, discomfort and distress for your patient which impacts on your ability to provide them with the care they need.1
NIV masks are commonly known to increase the chances of developing a pressure ulcer but are also vital to delivering quality respiratory care.2 It is therefore important to identify the risk factors associated with pressure ulcers and be confident in the steps you can take to prevent them.
Signs of a pressure ulcer developing can first be seen when the area on the patient’s skin in contact with the device becomes red and warm to the touch. There are four progressive stages as shown below:
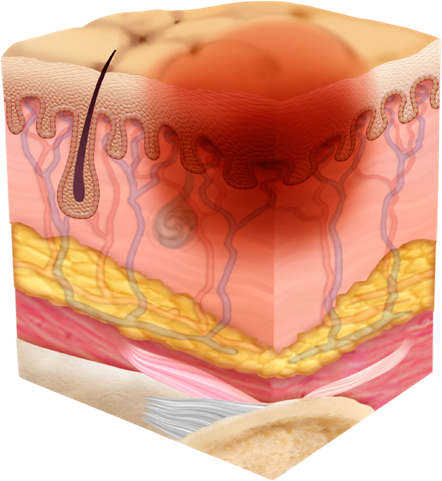
A localised red area that is warm to the touch. The term pressure injury is used as the skin is not yet broken in this stage.
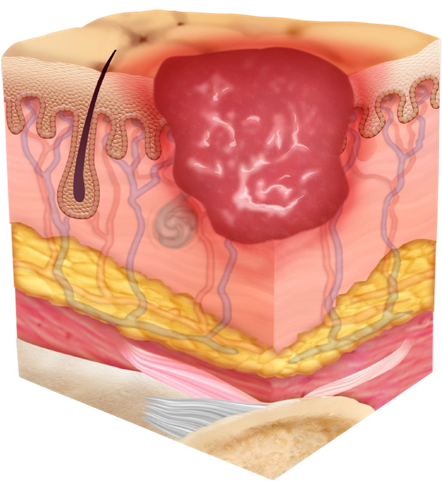
A pressure ulcer is visible as the skin is broken and partially lost.
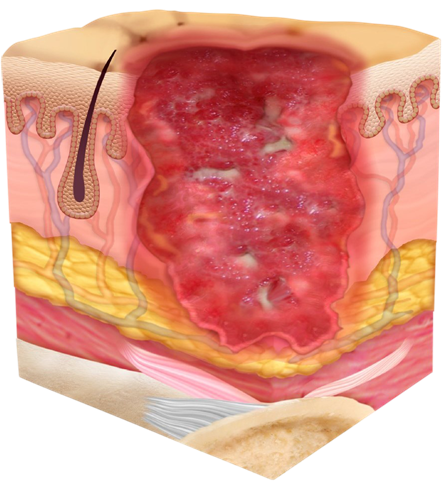
The pressure ulcer and tissue necrosis extends through all the skin layers. The underlying fat layer is also visible.
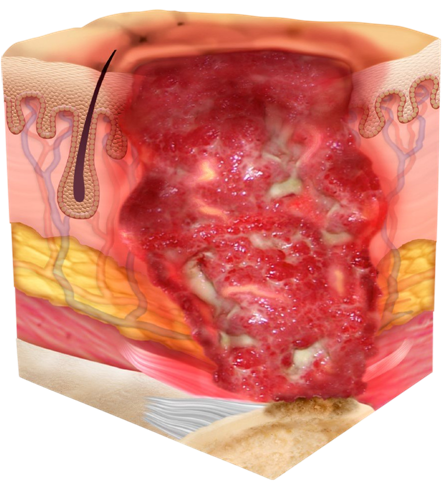
The pressure ulcer and tissue necrosis extends down to the fat, muscle and bone or cartilage.
In order for tissues to carry out their normal functions, they need a healthy supply of blood through blood vessels. Restrictions in blood flow to tissues have been found to contribute to the development of a pressure ulcer.
If skin is continuously rubbing on a surface, this can cause initial irritation. It can then develop into an abrasion wound. Shear forces between thin tissue and a hard surface pushing in opposing directions, such as sliding down a bed, can cause delicate vessels to stretch and tear resulting in the development of a pressure ulcer. 4
The skin and fat layers become thinner with old age or with poor nutrition due to reduced collagen and other components which keep the skin structurally sound. This makes bones protrude more. As a result, older and sicker patients are more prone to developing a pressure ulcer.1
NIV masks have been cited as one of the leading causes of pressure injuries in the ICU and, with respiratory failure ranking as one of the top patient conditions requiring admission into critical care, patients fitted with NIV masks are at an increased risk of developing pressure ulcers.2

A mask that is too big places unnecessary pressure on the face.
A mask that is too small causes unwanted friction.

Shifting the mask without loosening the straps pulls on the face causing unwanted friction and shear forces.

If the mask is not sitting symmetrically, it may place extra pressure on facial areas.
For NIV to work efficiently, leaks must be minimised, so it can be tempting to overtighten the mask. However, this increases the risk of a pressure ulcer developing as it places excess pressure on the face by the mask and straps.5
It is important to keep in mind that most modern ventilators can compensate for any leak that may occur and often do not require the mask to be heavily tightened.6
Contact points of the mask and headgear are areas to check for pressure ulcer formation.

Comfort is important to improve patient tolerance to NIV. Effective NIV therapy can help reduce time in the ICU and length of stay in the hospital.7
To help prevent the development of a pressure ulcer, finding the perfect balance between a good seal and a mask that does not apply too much pressure is fundamental for a quality patient experience.


Our NIV therapy solutions are thoughtfully designed with you and your patient in mind.