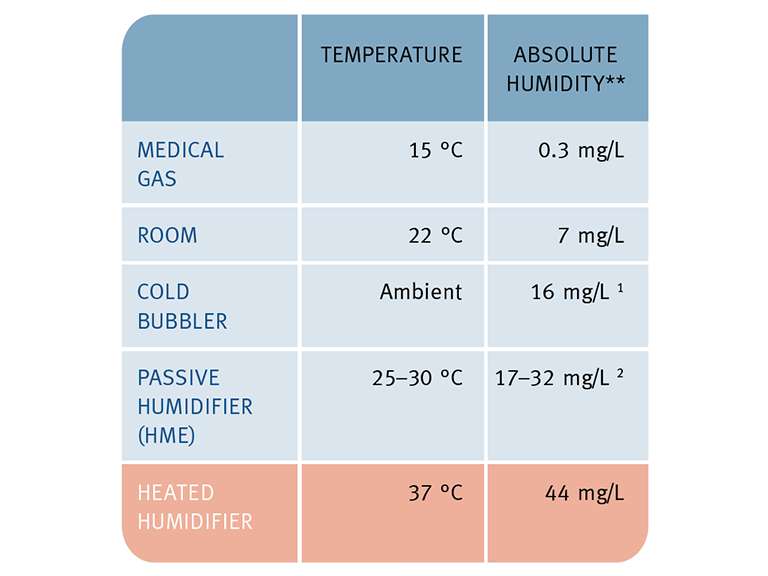
2. A Bypassed Airway
An endotracheal or tracheostomy tube bypasses the upper airway where the majority of humidification would naturally occur. The tube also bypasses the airway’s filtering mechanisms and compromises protective cough, gag and sneeze reflexes.
3. Higher Gas Flows
The respiratory mechanics of patients on noninvasive therapies change with potentially higher respiratory rates, larger tidal volumes and greater inspiratory flow rates. High gas flows are also required to deliver a number of therapies along the respiratory care continuum. These factors deplete the airway mucosa of heat and moisture. The airway mucosa will continue to lose heat and moisture to the gas flow, until the gas reaches body temperature, fully saturated.
These factors affect the function of the mucociliary transport system and can result in impaired airway defense and gas exchange.
Mucociliary Dysfunction
Medical gases, a bypassed airway and higher gas flows can have significant adverse effects.
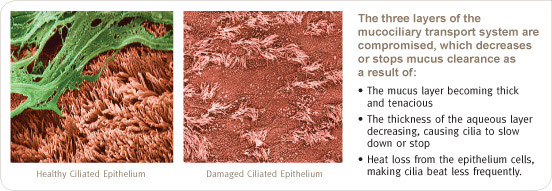
If the mucosa is exposed to low humidity for a long period of time, irreversible cell damage will occur. The lungs may already be compromised by pre-existing mucociliary dysfunction (e.g. due to age, smoking, chronic obstructive pulmonary disease (COPD), etc). To avoid further complications, provision of physiological levels of humidity becomes even more important for patients with these conditions.
Humidification allows the airway to maintain a natural balance of heat and moisture - optimizing gas exchange, lung defense and patient comfort.