Research interest in NHF is increasing. Over the past decade >350 publications per year (on average) have been cataloged on PubMed.
A significant number of controlled trials, systematic reviews and meta-analyses are included.
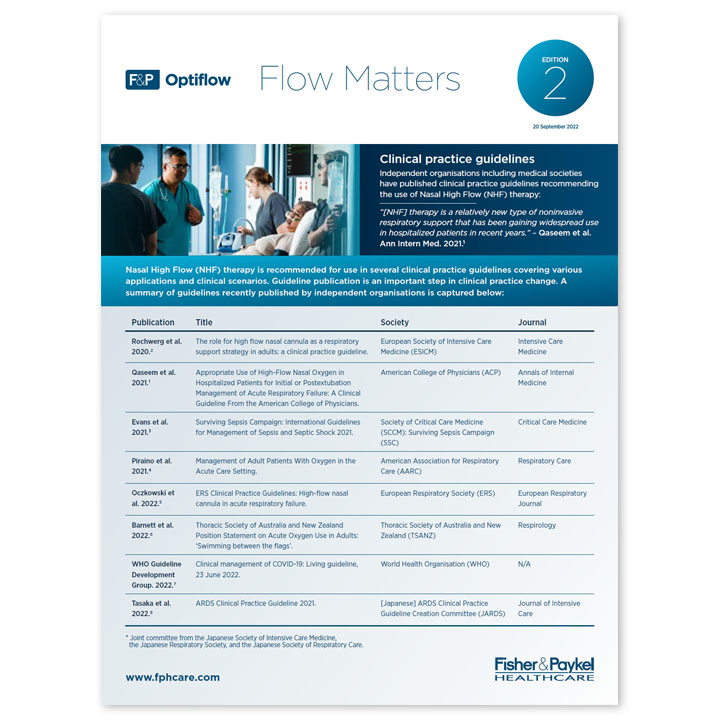
Medical societies around the world are now in a position to create recommendations that may change clinical practice.
| Clinical applications/ scenarios |
AARC Guideline 2021
AARC: Piraino et al. Management of Adult Patients With Oxygen in the Acute Care Setting. Respir Care. 2021 Nov 2:respcare.09294. doi: 10.4187/respcare.09294. Epub ahead of print. PMID: 34728574.
https://pubmed.ncbi.nlm.nih.gov/34728574/
|
ESICM Guideline 2020
ESICM: Rochwerg et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med. 2020 Dec;46(12):2226-2237. doi: 10.1007/s00134-020-06312-y. Epub 2020 Nov 17. PMID: 33201321; PMCID: PMC7670292.
https://pubmed.ncbi.nlm.nih.gov/33201321/
|
ERS Guideline 2022
Oczkowski et al. ERS clinical practice guidelines: high-flow nasal cannula in acute respiratory failure. Eur Respir J. 2022 Apr 14;59(4):2101574. doi: 10.1183/13993003.01574-2021. PMID: 34649974.
https://pubmed.ncbi.nlm.nih.gov/34649974/
|
SSC Guideline 2021
Evans et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021 Nov;47(11):1181-1247. doi: 10.1007/s00134-021-06506-y. Epub 2021 Oct 2. PMID: 34599691; PMCID: PMC8486643.
https://pubmed.ncbi.nlm.nih.gov/34599691/
|
WHO Guideline 2022
Clinical management of COVID-19: Living guideline, 23 June 2022. Geneva: World Health Organization; 2022 (WHO/2019-nCoV/Clinical/2022.1). Available from:
https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2022-1/ [Accessed 12 September 2022]
|
ACP Guideline 2021
Qaseem et al. Appropriate Use of High-Flow Nasal Oxygen in Hospitalized Patients for Initial or Postextubation Management of Acute Respiratory Failure: A Clinical Guideline From the American College of Physicians. Ann Intern Med. 2021 Jul;174(7):977-984. doi: 10.7326/M20-7533. Epub 2021 Apr 27. PMID: 33900796. https://pubmed.ncbi.nlm.nih.gov/33900796/https://pubmed.ncbi.nlm.nih.gov/33900796/
|
TSANZ Guideline 2022
Barnett et al. Thoracic Society of Australia and New Zealand Position Statement on Acute Oxygen Use in Adults: 'Swimming between the flags'. Respirology. 2022 Apr;27(4):262-276. doi: 10.1111/resp.14218. Epub 2022 Feb 17. PMID:
35178831. https://pubmed.ncbi.nlm.nih.gov/35178831/
|
JARDS Guideline 2022
Tasaka et al. ARDS Clinical Practice Guideline 2021 committee from the Japanese Society of Intensive Care Medicine, the Japanese Respiratory Society, and the Japanese Society of Respiratory Care Medicine. ARDS Clinical Practice Guideline 2021. J Intensive Care. 2022 Jul 8;10(1):32. doi: 10.1186/s40560-022-00615-6. PMID: 35799288; PMCID: PMC9263056. https://pubmed.ncbi.nlm.nih.gov/35799288/
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||