Neopuff™ T-piece resuscitator
Resuscitation masks
T-piece resuscitation circuits
While most babies born at term manage transition without significant medical intervention, about 10% may require assistance to begin breathing at birth and less than 1% need advanced neonatal resuscitation interventions.1-4
T-piece resuscitators are typically gas powered and capable of delivering a preset, consistent and controlled peak inspiratory pressure (PIP) and positive end-expiratory pressure (PEEP).
How does T-piece resuscitation work?
The T-piece connects to a face mask or other interface to deliver a flow-regulated, pressure-limited gas supply to the infant, enabling the application of controlled initial inflation breaths.
Consistent and controlled PIP and PEEP delivery help protect the lungs from injury and establish and maintain functional residual capacity (FRC). FRC is the volume of air that remains in the lungs following a typical expiratory phase. This volume is important for keeping the lungs open post exhalation and for ensuring adequate pulmonary gas exchange.5
Compared with other types of resuscitators, such as self-inflating bags and flow-inflating bags, T-piece resuscitators provide consistent and controlled pressures independent of operator experience.6,7
The International Liaison Committee on Resuscitation (ILCOR) international resuscitation guidelines recommend the use of a T-piece resuscitator when a gas source is available.8-10
T-piece resuscitation provides a range of benefits that ensure safe and effective respiratory support during neonatal resuscitation.
• Helps protect the lungs from injury
• Establishes and maintains FRC
• Heated and humidified T-piece resuscitation promotes normothermia
Helps protect the lungs from injury
T-piece resuscitators have been designed to provide consistent and controlled PIP during resuscitation.
PIP is the maximum inspiratory pressure required to improve oxygenation without causing adverse effects. Delivering a controlled PIP is important as uncontrolled PIP that is too high may lead to lung injury, while under-inflating the lungs may not provide adequate gas exchange.
At birth, the lungs of preterm infants are uniquely susceptible to injury because they are structurally immature, surfactant deficient, fluid filled, and unsupported by a stiff chest wall.
Animal studies have demonstrated that lung injury can occur during resuscitation with just a few large manual inflations.11,12 In immature animals, ventilation at birth with high tidal volumes associated with the generation of high PIP for a few minutes can cause lung injury, impaired gas exchange and reduced lung compliance.13
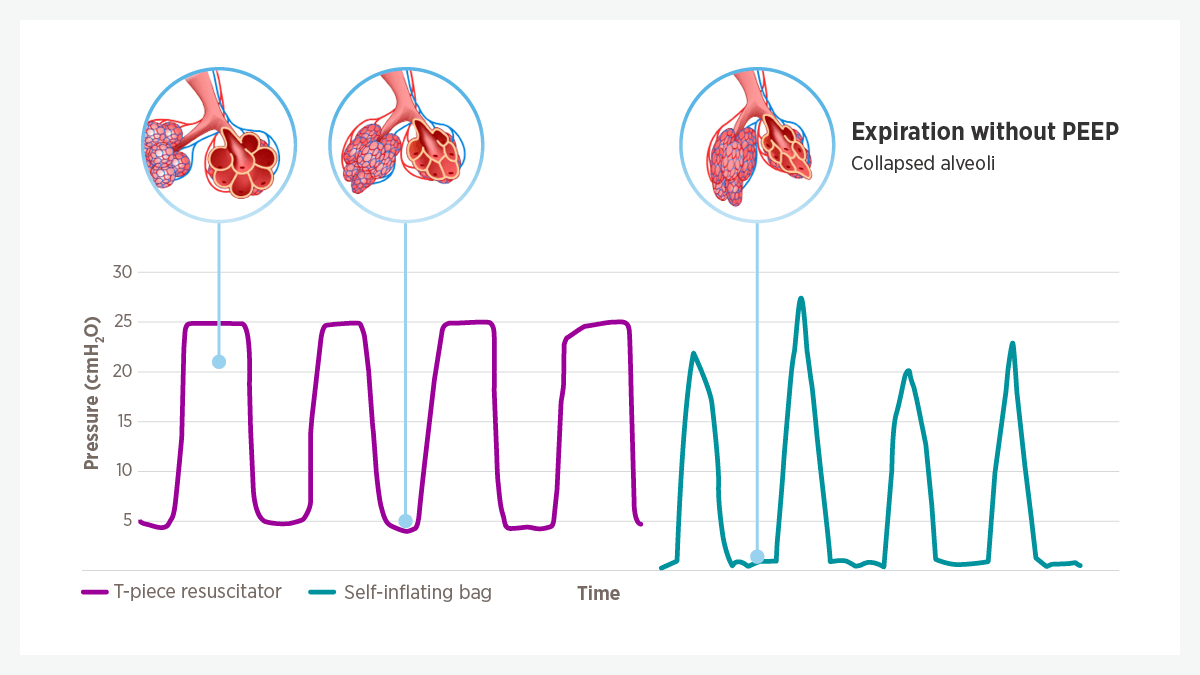
Fig 1. PEEP: peak end-expiratory pressure.
* Pressure measurements taken from a resuscitation simulator while a self-inflating bag and Neopuff were being used by a qualified resuscitator.
Establishes and maintains FRC
T-piece resuscitators deliver consistent and controlled PEEP, the residual pressure maintained at the end of expiration. Research suggests adequate levels of PEEP may help to establish and maintain FRC during transition at birth.14
Resuscitation guidelines recommend delivering PEEP whenever positive pressure ventilation is required in the delivery room.15 On a T-piece resuscitator, PEEP can be set to the desired pressure and tested before use on a patient.
Research has shown that providing PEEP early during ventilation improves the response to surfactant, and may also reduce delivery room intubation rates and the incidence of lung injury.16-18
Heated and humidified T-piece resuscitation promotes normothermia
Newborn infants are exposed to heat loss immediately following birth.
A meta-analysis found that the use of heated and humidified T-piece resuscitation in the delivery room resulted in significantly more infants with normothermia on neonatal intensive care unit (NICU) admission, compared with the use of cold, dry gas.19 Normothermia is defined as a rectal temperature between 36.5 °C and 37.5 °C.
The use of heated gas during delivery-room stabilization has also been observed to reduce the rate of moderate hypothermia on admission to the NICU, with no increased risk of hyperthermia.20
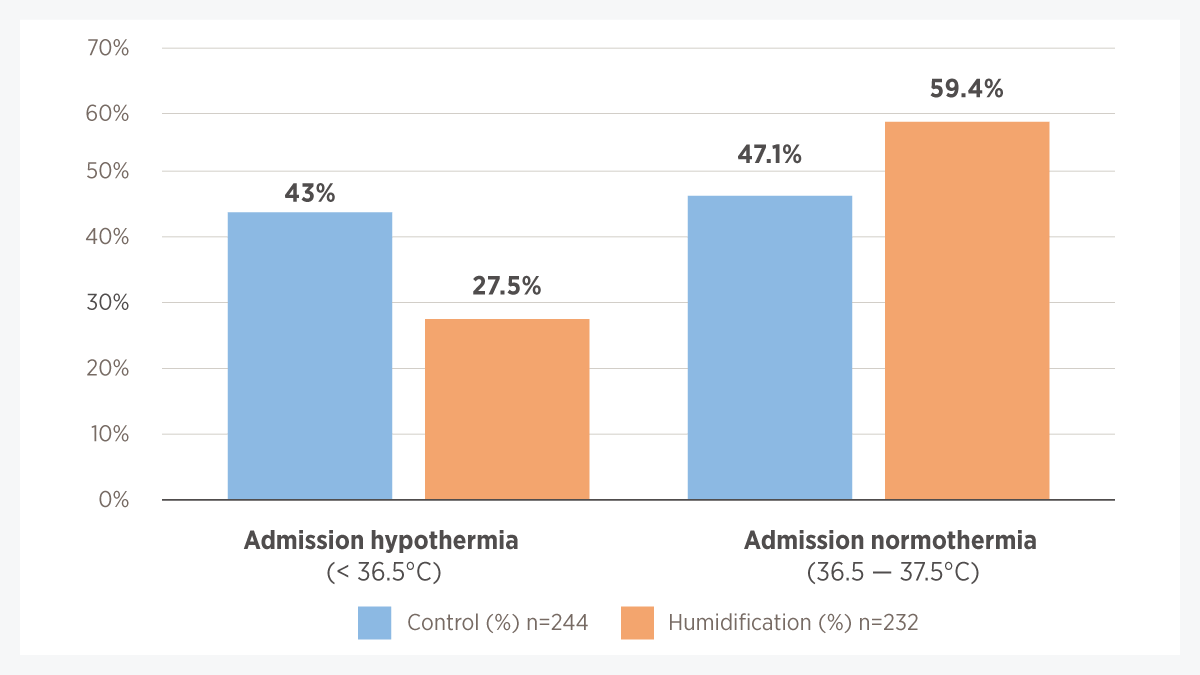
Fig 2. Heating and humidifying inspired gases for early stabilization of preterm infants resulted in a lower rate of hypothermia and a higher rate of normothermia on admission to the NICU when compared with no heating and humidification of inspired gases (control group).
Diagram adapted from Meyer, MP et al. Front Pediatr (2018).
.
F&P and Neopuff are trademarks of Fisher & Paykel Healthcare Limited. For patent information, see www.fphcare.com/ip