The journey to implement noninvasive therapies at the Rosie
This video explores research behind the decision to deliver CPAP and NHF at the hospital.

CPAP is a mode of noninvasive respiratory support that provides continuous distending pressure throughout the respiratory cycle to spontaneously breathing patients.
CPAP requires a closed system and is typically delivered using a nasal interface, circuit and a pressure generator (either a bubble generator or ventilator).
 | Intended to deliver prescribed pressure |
 | Interface designed to seal and maintain prescribed pressure |
 | Larger breathing tubes (compared to a standard oxygen cannula) lower resistance to flow |
| Establishes functional residual capacity1 | |
| Reduces the work of breathing1 | |
| Promotes gas exchange2 |

NHF is a mode of noninvasive respiratory support that provides high flows of heated and humidified blended air and oxygen through an unsealed interface.
NHF requires an open system and is typically delivered using an unsealed nasal high flow interface and a single-limb circuit. The flow range is dependent on the flow driver/platform used.
 | Delivers prescribed flow |
 | Interface designed to be unsealed |
 | Narrower breathing tubes (compared with CPAP) increase resistance to flow |
| Washes out anatomical dead space5 | |
| Reduces the work of breathing and improves oxygenation5,6 | |
| Improves patient comfort and tolerance to therapy7,8 |
| Continuous positive airway pressure | Nasal high flow |
| Provides continuous distending pressure throughout the respiratory cycle to spontaneously breathing patients. | Provides high flows of heated and humidified blended air and oxygen through an unsealed interface. |
| Requires a closed system and is typically delivered using a nasal interface, circuit and a pressure generator (either a bubble generator or ventilator). | Requires an open system and is typically delivered using an unsealed nasal high flow interface and a single-limb circuit. The flow range is dependent on the flow driver/platform used. |
| Interface | |
| Uses the FlexiTrunk interface | Uses the Optiflow Junior 2 interface |
| Intended to deliver prescribed pressure | Delivers prescribed flow |
| Interface designed to seal and maintain prescribed pressure | Interface designed to be unsealed |
| Larger breathing tubes, compared to a standard oxygen cannula, lowers resistance to flow | Narrower breathing tubes (compared with CPAP) increase resistance to flow |
| Primary mechanisms | |
| Establishes functional residual capacity1 | Washes out anatomical dead space5 |
| Reduces the work of breathing1 | Reduces the work of breathing and improves oxygenation5,6 |
| Promotes gas exchange2 | Improves patient comfort and tolerance to therapy7,8 |
| Choose when you want to: | |
| Set and control pressure | Set and control the flow rate |
| Stent open lungs and airway | Generate a low level of pressure |
| Reduce the need for mechanical ventilation3 | Reduce nasal trauma9 |
| Decrease the incidence of bronchopulmonary dysplasia4 | Decrease re-breathed CO2 |
CPAP continues to be the standard of care in neonates < 28 weeks' gestational age (GA). However, there are several pathways of care in which CPAP and NHF may be used.
Postextubation
support
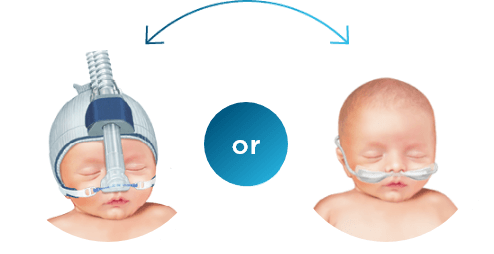
CPAP or NHF
Wilkinson et al. 2016
Cochrane Review
Primary respiratory support
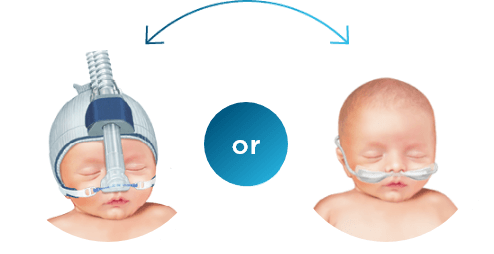
CPAP or NHF
Bruet et al. 2021
Systematic Review
Alternative to prolonged CPAP
CPAP or NHF
Roehr et al. 2016, Yoder et al. 2017 Consensus
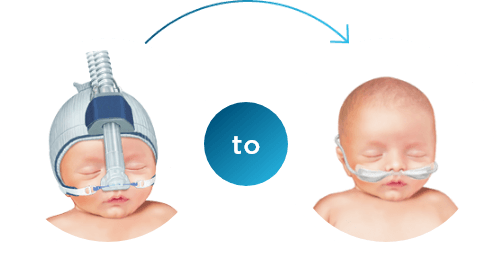
| < 28 weeks' GA CPAP first For neonates with compromised lung development and a higher need for respiratory support. |
| From 28 weeks' GA NHF first with rescue CPAP This approach may be considered for neonates who are stable or require lower acuity of care because it provides two noninvasive options before mechanical ventilation needs to be taken into consideration. |
.
F&P, FlexiTrunk and Optiflow are trademarks of Fisher & Paykel Healthcare Limited. For patent information, see www.fphcare.com/ip