What is a pressure ulcer?
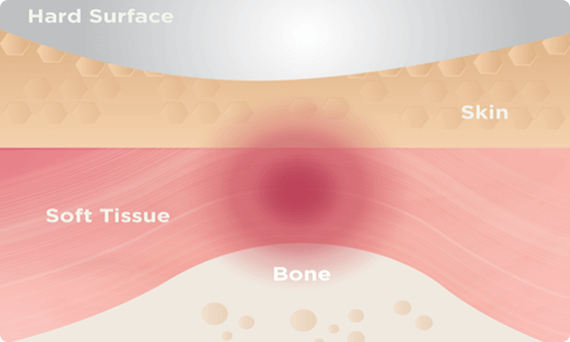
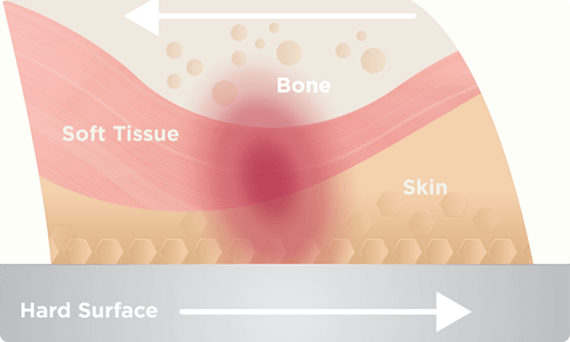
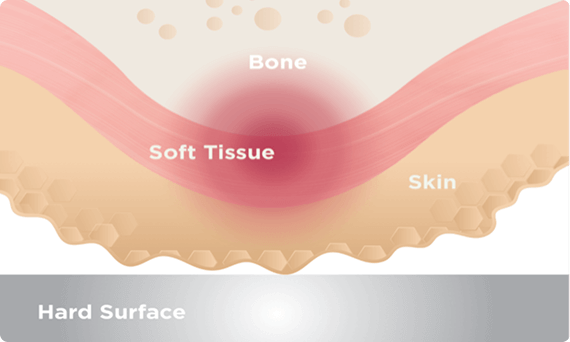
A pressure ulcer, also known as a pressure sore or injury, is localized damage to the skin and underlying tissues. These ulcers often develop on areas where thin tissue covers bony parts of the body that are in contact with hard surfaces such as beds and medical devices.1
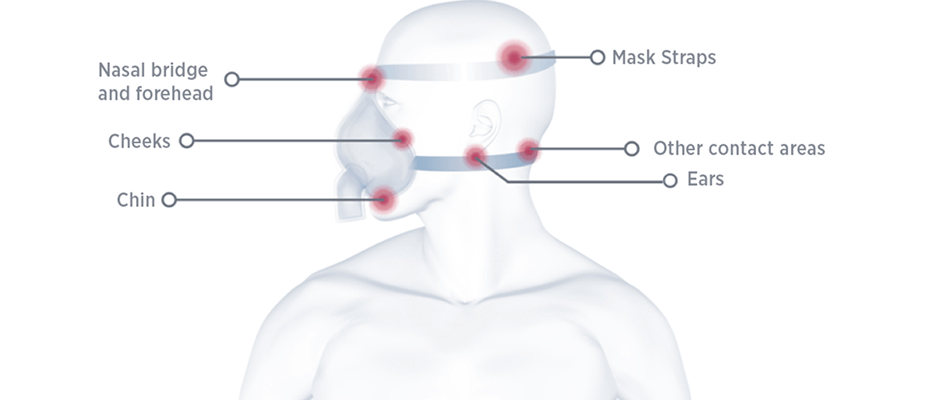
Using medical devices such as masks or breathing tubes for extended periods increases the risk of pressure ulcers. This can cause pain, anxiety and discomfort for patients, which can impact the quality of care provided.1
NIV masks, while essential for respiratory care, can also increase the risk of pressure ulcers.2 Therefore, it is important to identify risk factors and be confident in the steps to take to prevent them.
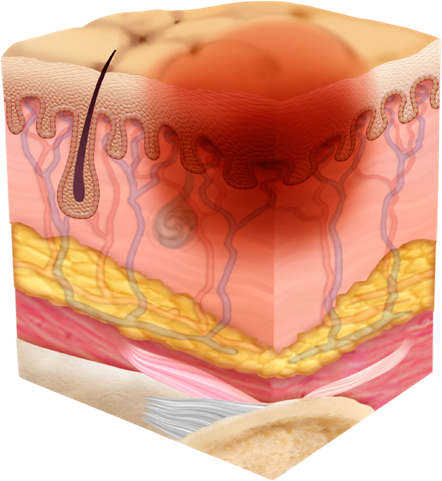
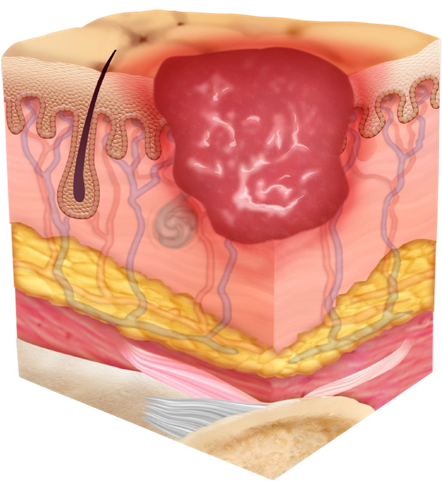
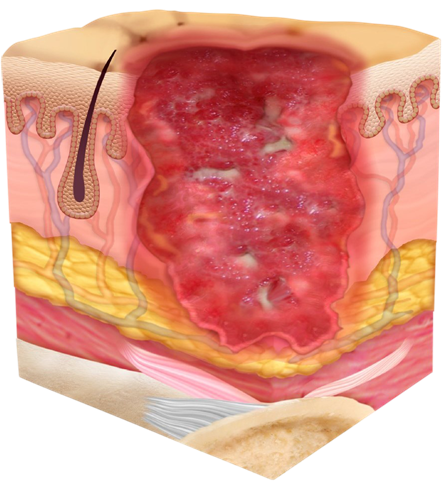
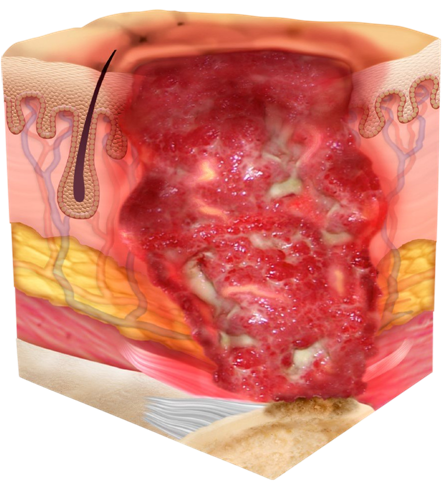
Signs and Stages of a Pressure Ulcer
Pressure ulcers develop progressively through four distinct stages: