1.
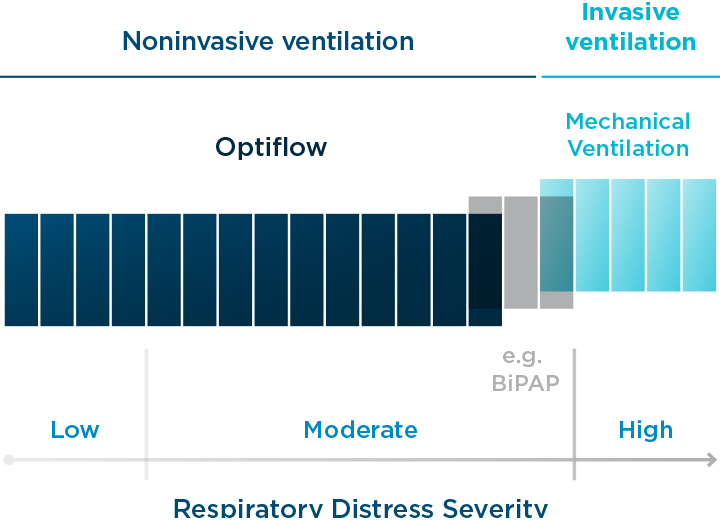
Nasal High Flow (NHF) is a form of noninvasive (NIV) respiratory therapy, but it is not a ventilator or a CPAP device.
Watch below to compare NHF and NIV. Learn about how Nasal High Flow can be used as a ‘multitool’ of respiratory support.
2.
NHF is called many things, High flow nasal cannula (HFNC), high-flow therapy (HFT), high-flow oxygen/therapy (HFO/T), nasal high flow (NHF), or just plain high flow (HF).
Our preferred generic descriptor is nasal high flow because it’s all about nasal delivery of high flows of humidified air.
Commercially, we call it Optiflow™ nasal high flow therapy which can be delivered in several different ways, i.e., there are several devices you can use to provide Optiflow NHF therapy.
3.
Optiflow can deliver high levels of oxygen (from no added oxygen, i.e., 21% FiO2 up to 100%), but NHF therapy is significantly more sophisticated than that.
The higher rates of flow (independent of oxygen) confer benefits that oxygen alone cannot, i.e., reduction of dead space and dynamic, positive airway pressure, both of which can increase alveolar ventilation.
4.
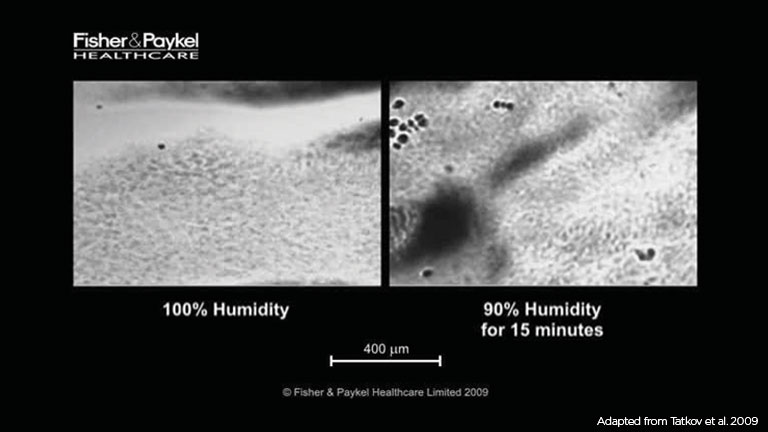
A fundamental element of NHF therapy is airway hydration, i.e., heated humidification.
Heating and humidifying not only make high gas flows tolerable but also prevent desiccation of the airway epithelium and maintain and improve mucociliary clearance (MCT).
Your MCT system is fundamental in protecting your vulnerable airways and lungs - it's not just about comfort.
Watch the MCT system in action on the right - turn the audio on.

5.
NHF is indicated for a broad range of patients, but it is fundamentally designed to treat patients with respiratory compromise, i.e., those experiencing:
- High respiratory rate
- Dyspnea
- High work of breathing
- Low SpO2
- High PaCO2
You might also be interested in how quickly NHF works.
6.
Guidelines and recommendations for the use of NHF are emerging.
An ever-increasing body of evidence has allowed medical societies worldwide (including AARC, ESICM, and ERS) to create guidelines and make recommendations for the use of NHF compared to other forms of NIV and conventional oxygen therapies.
The guidelines include the use of NHF for:
- Acute hypoxemic respiratory failure (AHRF)
- Patients with severe or critical COVID-19
- High-risk post-operative patients
- Pre-oxygenation for peri-intubation patients
- Low-risk, extubated patients
- High-risk, extubated patients
- NIV-rested AHRF patients
- etc.
7.
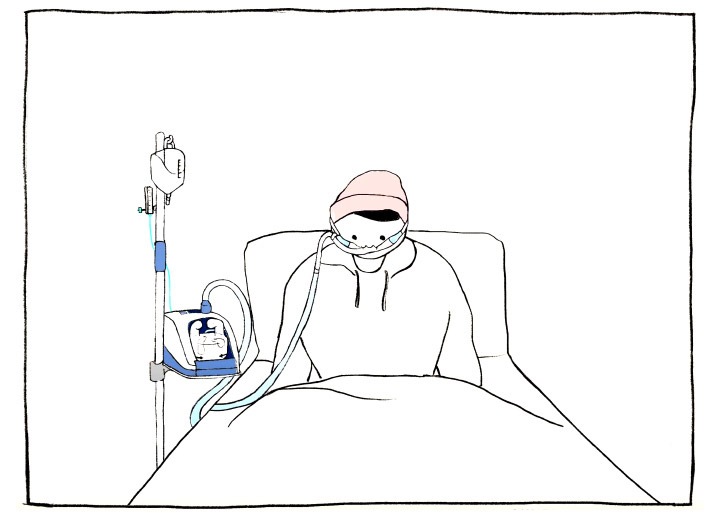
Compared with other NIV modalities, NHF has the distinct advantage of being delivered via a cannula (or tracheotomy) rather than a mask.
There are several benefits:
1. a mask seal is not required, making setup a more straightforward process,
2. it's proven to be more comfortable, which may encourage therapy compliance
3. a smaller, less intrusive interface may facilitate better communication with caregivers and loved ones.
7.
Compared with other NIV modalities, NHF has the distinct advantage of being delivered via a cannula (or tracheotomy) rather than a mask.
There are several benefits:
1. a mask seal is not required, making setup a more straightforward process,
2. it's proven to be more comfortable, which may encourage therapy compliance
3. a smaller, less intrusive interface may facilitate better communication with caregivers and loved ones.