A newborn’s respiratory system is reliant on humidity to maintain physiological balance, assist natural defense mechanisms, and conserve energy for growth and development.
The benefits of delivering heated and humidified gases during all forms of respiratory support is well recognized from research 1-4 and clinical practice.5-6
• What is humidity?
• Three vital reasons why humidification is important
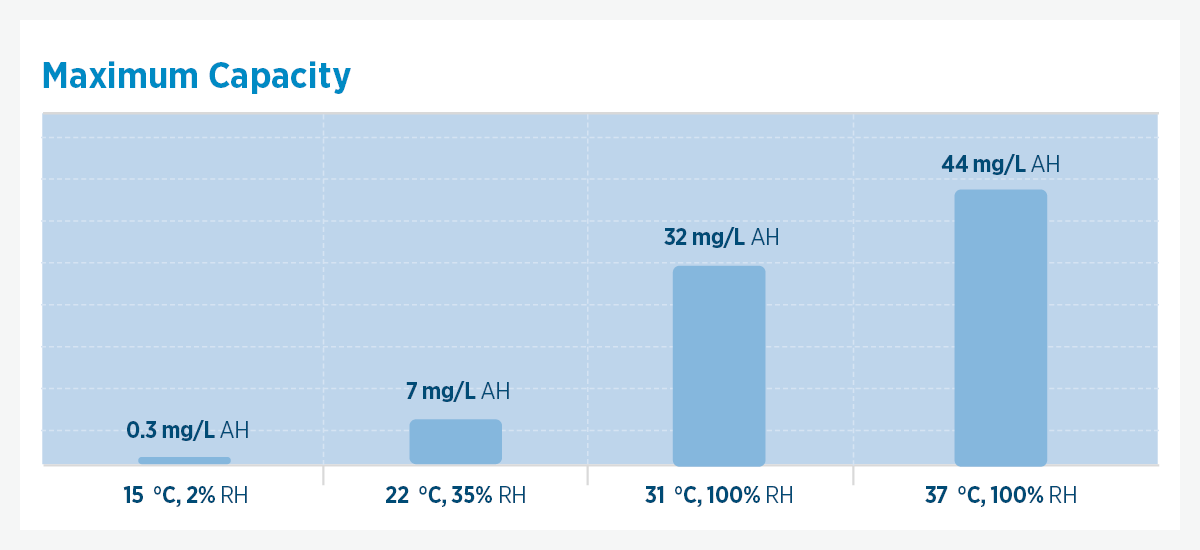
Absolute humidity (AH) represents the total amount of water vapor in a given volume of gas in which it is contained. AH is measured as mass divided by volume of gas (mg/L).
If the water held in a liter of gas was condensed and weighed in milligrams, the absolute humidity of the gas would be measured in milligrams per liter of gas.
Relative humidity (RH) takes in the water contained in the gas, compared with how much water it can hold before the vapor condenses to liquid water. RH is measured as a percentage.
100% RH: If the same volume of gas holds 44 mg of water vapor, it is full or saturated with water vapor, so its RH is 44 mg / 44 mg or 100% RH.
25% RH: If a liter of gas holds a maximum 44 mg of water vapor, it will be a quarter full and contain only 11 mg of water vapor, so its RH is 11 mg / 44 mg or 25% RH.
Water vapor, viruses, bacteria and nebulized liquid water all have different particle sizes.
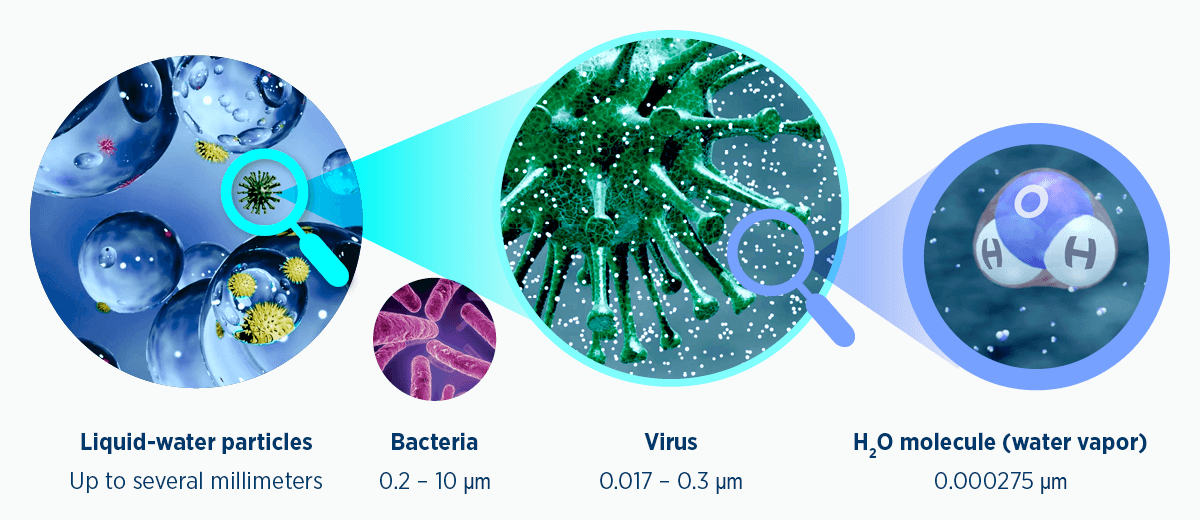 Fig 4. Relative sizing of common pathogens to water in both liquid and gas states. μm, micrometers (microns); 1 mm = 1,000 μm.
Fig 4. Relative sizing of common pathogens to water in both liquid and gas states. μm, micrometers (microns); 1 mm = 1,000 μm.

Assists the body’s natural defense mechanisms in the airway
The primary defense mechanism: Reflexes such as sneezing, coughing and gagging are supported by the natural filtration of nasal hairs and the upper airway. In preterm infants, these mechanisms can be underdeveloped.13-15
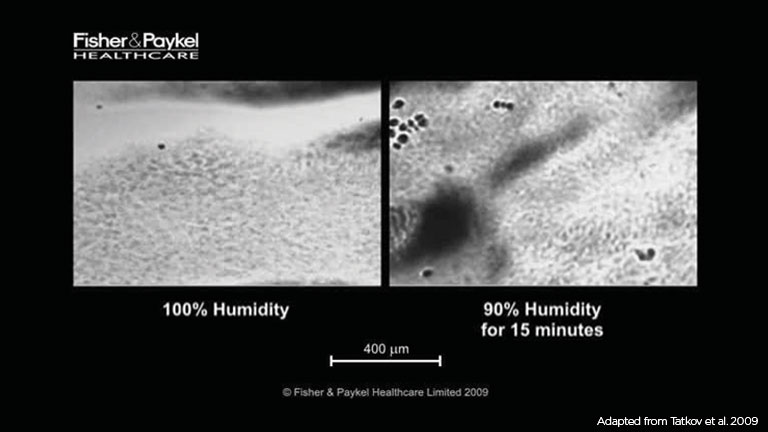
Mucociliary transport – the second line of defense: The role of the mucociliary transport system is to trap inhaled contaminants (in mucus) and transport them up and out of the airway. The efficiency of this mechanism is reliant on several factors, including the temperature and humidity of inspired gas.16,17
The lower the humidity of the inspired gas, the further it needs to travel down the airway before physiological temperature and humidity are reached.18

At birth, newborns are exposed to immediate cold stress and heat loss. Premature infants may also have limited heat production capabilities, along with an increased need to conserve limited energy reserves.19
Infants need energy for growth and development. Therefore, assisting in thermoregulation is important. There is a range of interventions such as ensuring a neutral thermal environment, drying towels and blankets, a radiant warmer, or skin-to-skin contact.
Humidifying delivered therapies is important also, to promote conservation of energy. When inadequate levels of humidity are inhaled, water vapor is drawn from the airway mucosa until the inspired gas has reached 37 °C, 44 mg/L H2O. The energy cost to the infant for each gram of water removed from the mucosa is 0.58 cal (2.4 j).19

In addition to assisting natural defense mechanisms in the airway and promoting conservation of energy for growth and development, adequate humidification during respiratory support has been found to increase patient comfort and therapy tolerance.4,20-23
While this data is derived predominantly from adult patients, the principles are applicable to the pediatric population.24-26 In particular, humidification is associated with the clearance of retained secretions and prevention of airway drying, which may subsequently improve lung compliance and the work of breathing.27-29
The F&P 850™ System unites the delivery of heated humidification with clinical usability and the reduction of mobile circuit condensate. Clinically tested, clinically beneficial, clinically proven.
An effective and versatile solution for delivering Optiflow nasal high flow. Larger-sized Optiflow™ Junior 2/2+ nasal interfaces can be combined with the Airvo™ 2 for a complete Optiflow system.
Enhanced usability. Minimized condensation. Advanced protection. The F&P 950™ is a premium performance humidification system that delivers many benefits to patients and healthcare providers.
Provides compatibility with a wide range of Optiflow interfaces (down to Optiflow Junior 2 Medium), features an integrated battery for intra-hospital transport and offers both direct and low pressure oxygen-input methods.

F&P, F&P 950, Airvo and Optiflow are trademarks of Fisher & Paykel Healthcare Limited. For patient information, see www.fphcare.com/ip